Can You imagine the revenue cycle you deserve?
Learn more about the features ImagineSoftware offers to optimize the revenue cycle from point-of-service to zero balance.
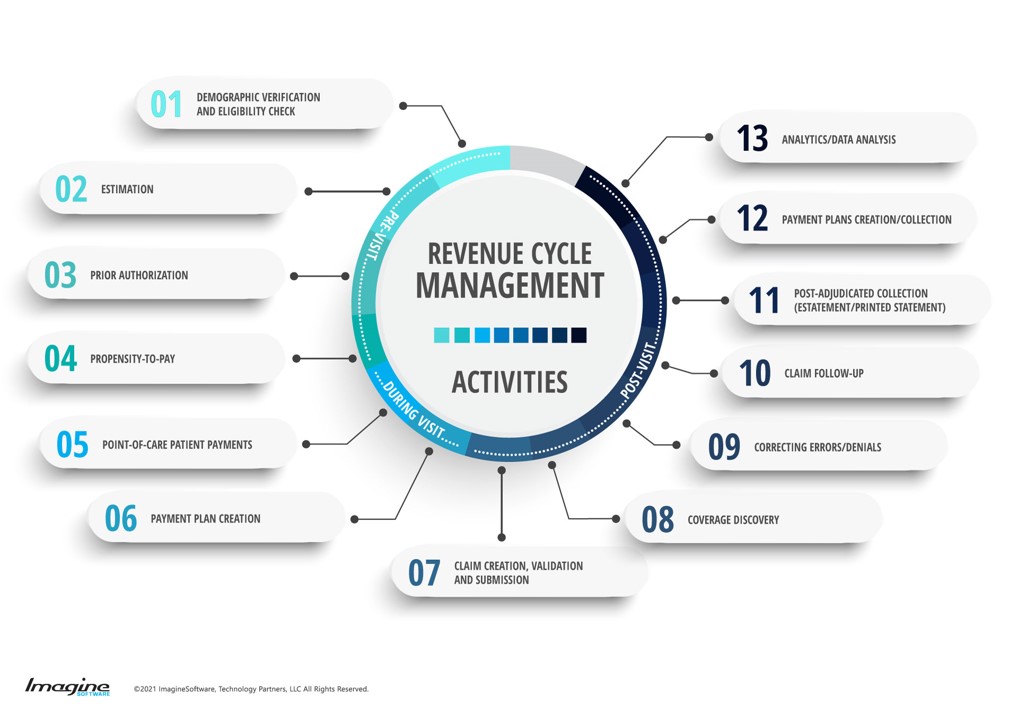
What is RCM automation?
ImagineSoftware uses machine learning to reduce the time spent between labor-intensive tasks such as demographic verification, collections and reporting. Benefits include more first pass acceptance on claims, better staff efficiency, and 95% of your payment posting performed with zero human intervention.
Read MoreWhat challenges can RCM automation solve?
-
“I’m tired of manually generating and submitting claims”
Hands-free claims generation and submission. Minimal human intervention.
-
“I’ve outgrown my current platform”
Technology that evolves with your business. For those who need to scale their operations.
-
“I’m fed up with managing multiple billing vendors”
Replace multiple systems from mergers and acquisitions with one platform across specialties.
-
“I don’t have the budget to change billing systems”
Free up the time of FTEs while keeping the same productivity with robotic process automation.
Gain efficiency in your billing cycle using configurable workflows.
| STAGE IN BILLING CYCLE | AVG PREVIOUS SOFTWARE PROVIDER | |
|---|---|---|
| Date of Service to Date posted | 8.2 days | 4.7 days |
| Date Posted to HCFA Creation | 13.48 days | 1.23 days |
| HCFA Filed to First Payment | 30.66 days | 16.53 days |
| Charge Posted to Claims Release | 13.48 days | 1.51 days |
| Charge Posted to Claims Filed | 13.48 days | 2.47 days |
| Charge Posted to First Payment | 53.32 days | 18.98 days |
Improve Your Billing Efficiency By:
Multi-Specialty Billing Software
Go Completely Paperless
Propensity to Pay
Electronic Remittance and Submission
Maximize Staff Capability
"I can get through an entire day’s payment posting in 30 minutes."