Your Guide to the Revenue Cycle Management Workflow
In the dynamic realm of healthcare administration, the mastery of revenue cycle management software stands as a cornerstone of financial and operational success. This pivotal process is a comprehensive journey, beginning with patient registration and culminating in final payment – one where every step’s accuracy and timeliness matters profoundly. The revenue cycle process is not just a financial pathway; it is a reflection of the healthcare institution's commitment to precision, efficiency, and patient-centered care.
The initial stage of patient registration is much more than filling out forms. It sets the tone for the entire cycle, establishing a framework for financial interactions and patient responsibility. This stage's accuracy and clarity are critical, ensuring a smooth transition to the subsequent phases of coding and billing. Here, the fusion of medical knowledge and financial acumen comes to the fore, where services rendered are translated into the language of billable entities. This translation is more than mere numbers; it represents an understanding of patient care and the meticulous attention to detail necessary for accurate billing.
As we navigate further into the revenue cycle, the complex world of claims management and payment processing unfolds. This phase is the embodiment of the process's intricacy, demanding an in-depth understanding of diverse payer regulations and the stringent adherence to compliance standards. It's about striking a balance between securing timely reimbursements and maintaining unwavering dedication to patient care.
Technology's role in elevating the revenue cycle is undeniable. Cutting-edge software solutions are redefining the financial operations within healthcare, introducing levels of streamlining and precision once thought unattainable. These technological advancements are not just about efficiency; they represent a shift towards a more patient-focused approach, where the financial elements are handled with such finesse that healthcare providers can devote much more attention to patient care.
Thus, the revenue cycle process is integral to the financial health of healthcare institutions. It is a complex, yet indispensable system that ensures uninterrupted high-quality care supported by a robust financial backbone. Grasping its intricacies is crucial for navigating the financial landscape of the healthcare industry.
What is RCM in Healthcare?
Exploring what is RCM in healthcare unveils a critical process integral to the financial health of healthcare institutions. Revenue Cycle Management (RCM) encompasses various stages from patient appointment scheduling to the final act of payment collection. This multifaceted process ensures that healthcare services are compensated effectively, balancing financial viability with patient care.
How Does RCM Enhance Healthcare Administration?
-
Patient Scheduling and Registration
It starts with precise data collection, crucial for setting the right course for the entire revenue cycle. -
Treatment and Documentation
Accurate documentation of treatments is vital for billing and forms the basis of the claims. -
Medical Coding and Billing
Converting services into standardized codes for insurance communication is a pivotal part of RCM. -
Claims Submission and Follow-Up
Efficient handling of claims, including tracking and addressing denials, is crucial for financial fluidity. -
Payment Collection
The cycle culminates in collecting payments, necessitating robust systems for both insurance and patient payments.
A significant aspect of RCM involves the accurate capture and processing of patient information. Verifying insurance coverage and securing necessary authorizations are key to reducing claim denials and accelerating reimbursements.
Medical coding and billing, integral to RCM, requires an in-depth understanding of medical terminologies and coding standards. The accuracy in this phase is directly proportional to the efficiency of the revenue cycle.
The role of proactive claims management in RCM cannot be overstated. This includes not just the diligent tracking of claims but also the analysis of data for process improvements. Identifying patterns in claim denials and enhancing patient payment methods are part of this continuous improvement process.
In essence, RCM in healthcare is a crucial component that intertwines the financial and patient care aspects of healthcare administration. Effective management of this cycle is vital for the operational success and sustainability of healthcare providers.
Imagine has taken the administrative headaches of practice management off my plate, giving me more time to be a pathologist.
What is RCM Workflow?
Understanding the RCM workflow is pivotal for any healthcare provider looking to streamline their financial operations. The question, what is RCM workflow, leads to a comprehensive view of the series of actions and procedures involved in managing the financial aspects of patient care, from the initial patient interaction to the final payment collection. It's a critical component for maintaining financial stability and efficiency within healthcare organizations.
Essential Elements of an Efficient RCM Workflow
-
Initial Patient Interaction
This crucial first step involves gathering and verifying patient information, setting the stage for all subsequent financial transactions. -
Service Documentation
Accurate and thorough documentation of services provided is vital for the next steps in the billing process. -
Medical Billing Process Steps
This includes translating the documented services into standardized billing codes, a process that requires meticulous attention to detail. -
Claims Submission
After coding, claims are prepared and submitted to insurance companies, marking a critical point in the revenue cycle. -
Payment Processing
This involves tracking the claims, processing payments from insurers, and handling patient billing. -
Account Reconciliation
The final stage, where all financial transactions are reviewed, ensuring accuracy and completeness.
In an effective RCM workflow, the revenue cycle plan plays a foundational role. It outlines the strategic approach to each step in the cycle, ensuring consistency and efficiency. This plan must be dynamic, adaptable to changes in healthcare regulations and patient needs.
Accuracy in the medical billing process steps is of paramount importance. Errors in coding or documentation can lead to claim denials, resulting in financial losses and administrative burdens. Therefore, continuous training and updating of coding knowledge are essential for maintaining an effective RCM workflow.
Moreover, RCM workflows are not static; they require ongoing analysis and optimization. Regular auditing and performance assessments help in identifying bottlenecks and areas for improvement, such as:
- Enhancing patient communication and information collection.
- Streamlining coding and billing processes for efficiency.
- Implementing advanced software solutions for automation and accuracy.
- Developing strategies to reduce claim denials and expedite payments.
- Fostering a culture of continuous improvement among staff.
A robust RCM workflow is integral to the successful management of a healthcare provider’s financial health. It is a complex, yet essential system that intertwines financial stability with patient-focused care. Mastery of this workflow is crucial for any healthcare organization aspiring to excel in today's dynamic healthcare landscape.
How to Learn Revenue Cycle Management
For healthcare organizations and professionals, understanding how to learn revenue cycle management is essential. This knowledge not only enhances financial performance but also contributes significantly to patient satisfaction and overall operational efficiency. Revenue Cycle Management (RCM) is a complex field, and gaining proficiency in it involves understanding various components, from patient registration to final payment collection.
Key Steps to Mastering RCM
-
Educational Resources
Utilize online courses, webinars, and workshops focused on RCM. Many of these resources are tailored to different levels of experience, from beginners to advanced professionals. -
Professional Training Programs
Enroll in specialized training programs offered by healthcare management organizations or institutions. These programs often provide comprehensive knowledge and hands-on experience. -
Industry Conferences and Seminars
Attend industry-specific events to learn about the latest trends, technologies, and best practices in RCM. -
Networking with Professionals
Connect with experienced RCM professionals through networking events or online platforms. Peer learning and mentorship can provide valuable insights into real-world applications of RCM principles. -
Hands-On Experience
Gaining practical experience through internships or working in healthcare administration is invaluable. Direct involvement in RCM processes offers a deeper understanding of the challenges and intricacies involved. -
Continuous Learning and Adaptation
Stay updated with the latest regulations, technology advancements, and industry changes. The healthcare field is ever-evolving, and so are the practices in revenue cycle management.
Medical Billing Cycle is a crucial component of RCM training and development. It involves understanding how medical services are coded, billed, processed, and followed up. Proficiency in medical billing requires familiarity with coding standards, payer policies, and patient billing procedures. Regular updates and training in these areas are crucial as they frequently change.
In addition, leveraging technology is a key aspect of modern RCM. Understanding how various software and tools can automate and optimize different stages of the revenue cycle is vital. Many platforms offer analytics and reporting features, providing valuable insights for improving financial performance.
I feel like we are more partners than customers, ImagineSoftware wants us to succeed.
Read the full Case Study, Funneling All Specialties through One Billing Software, here
Learning RCM is a continuous journey that requires dedication and a proactive approach. It’s about combining knowledge with practical application, staying adaptable, and always looking for ways to improve processes and outcomes. For anyone in the healthcare field, mastering RCM is not just about managing finances; it’s about contributing to the overall success and sustainability of the healthcare system.
How Many Stages are There in RCM?
A key question for healthcare providers aiming to optimize their operations is, "How many stages are there in RCM?" Understanding the number and nature of these stages is crucial for effectively managing the revenue cycle. Revenue Cycle Management (RCM) in healthcare is a multifaceted process, with each stage playing a critical role in ensuring financial stability and operational efficiency.
The Stages of Revenue Cycle Management
- Patient Pre-Registration: This initial stage involves gathering patient demographic and insurance information before their visit.
- Registration: At the point of service, additional information is collected, and financial responsibility is communicated to the patient.
- Charge Capture: Medical services provided to the patient are translated into billable charges.
- Claim Submission: These charges are then compiled into a claim, which is submitted to the insurance company for reimbursement.
- Remittance Processing: After the insurance company processes the claim, they send remittance advice detailing what will be paid.
- Insurance Follow-Up: This involves addressing any issues with insurance payments, such as denials or partial payments.
- Patient Billing and Collections: Any remaining balance after insurance is billed to the patient, and efforts are made to collect this balance.
- Denial Management: This stage deals with analyzing and appealing any denied claims.
- Reporting: Regular financial reporting helps in analyzing the overall performance of the RCM process.
Each stage of the RCM process, from patient pre-registration to final reporting, is interconnected, requiring a seamless flow of information and efficient management.
Revenue cycle steps are designed to maximize revenue collection while minimizing delays and errors.
The efficiency of each stage impacts the overall effectiveness of the revenue cycle. For instance, accurate charge capture and proper claim submission are vital for reducing claim denials and delays in payments. Similarly, efficient patient billing and collection processes are essential for maintaining cash flow.
Understanding and optimizing these stages are key for any healthcare provider. It involves not just following each step meticulously but also regularly reviewing and improving the processes. Effective RCM results in quicker payment turnarounds, reduced claim denials, and overall improved financial health for the healthcare provider.
What are the 13 Steps of the Revenue Cycle?
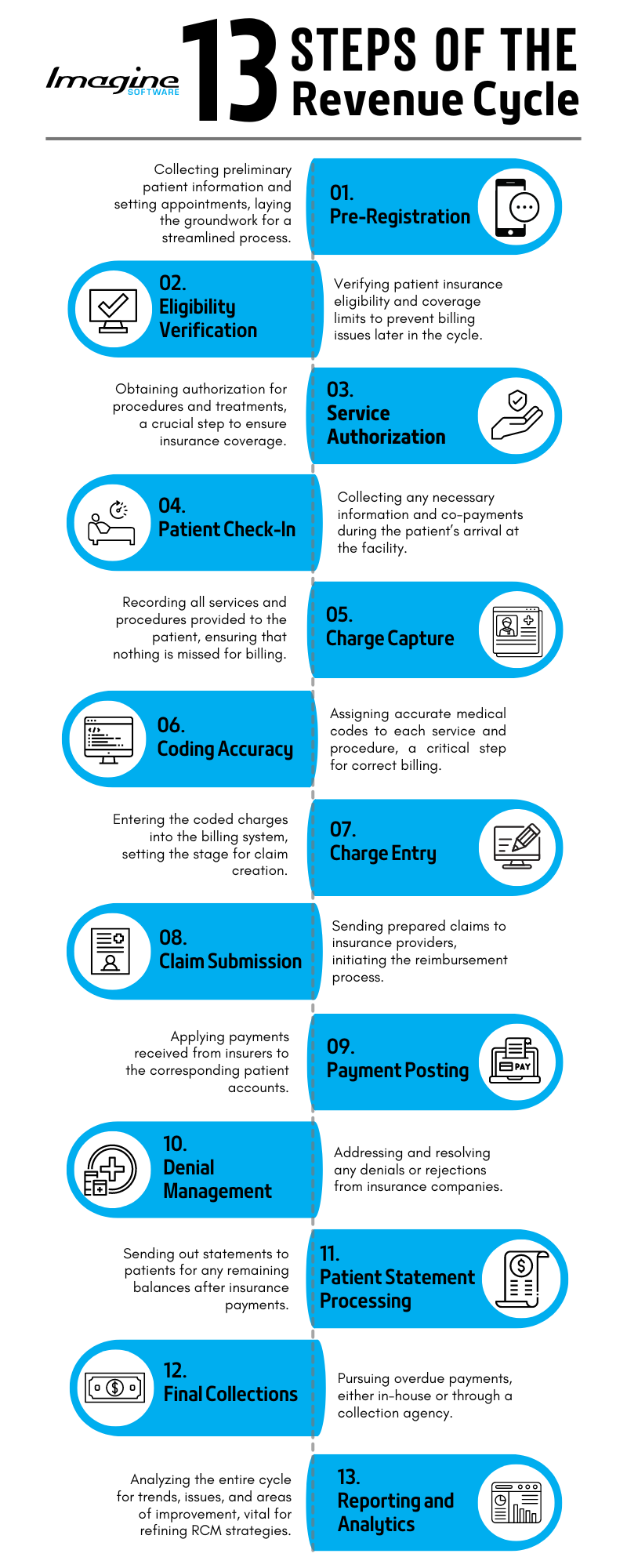
Exploring the 13 steps of the revenue cycle reveals a detailed and intricate process critical to the financial health of healthcare providers. Each step in the Revenue Cycle Management (RCM) process represents a unique and essential component of the entire financial journey, from patient entry into the system to the final reconciliation of accounts.
[flowchart infographic of 13 steps with corresponding keywords]
Detailed Overview of the 13 Steps in RCM
- Pre-Registration: This involves collecting preliminary patient information and setting appointments, laying the groundwork for a streamlined process.
- Eligibility Verification: Verifying patient insurance eligibility and coverage limits to prevent billing issues later in the cycle.
- Service Authorization: Obtaining authorization for procedures and treatments, a crucial step to ensure insurance coverage.
- Patient Check-In: Collecting any necessary information and co-payments during the patient’s arrival at the facility.
- Charge Capture: Recording all services and procedures provided to the patient, ensuring that nothing is missed for billing.
- Coding Accuracy: Assigning accurate medical codes to each service and procedure, a critical step for correct billing.
- Charge Entry: Entering the coded charges into the billing system, setting the stage for claim creation.
- Claim Submission: Sending prepared claims to insurance providers, initiating the reimbursement process.
- Payment Posting: Applying payments received from insurers to the corresponding patient accounts.
- Denial Management: Addressing and resolving any denials or rejections from insurance companies.
- Patient Statement Processing: Sending out statements to patients for any remaining balances after insurance payments.
- Final Collections: Pursuing overdue payments, either in-house or through a collection agency.
- Reporting and Analytics: Analyzing the entire cycle for trends, issues, and areas of improvement, vital for refining RCM strategies.
Each of these steps is an integral part of a successful RCM process. For example, precise charge capture and coding accuracy are vital for avoiding claim denials. Efficient claim submission and payment posting ensure a steady cash flow, while proactive denial management and patient statement processing are crucial for maintaining financial stability.
In-depth knowledge and mastery of these 13 steps are essential for healthcare providers to navigate the complex financial landscape effectively. These steps, when executed well, not only secure financial viability but also enhance patient satisfaction by providing clarity and transparency in billing.
Navigating the complexities of Revenue Cycle Management (RCM) is essential for healthcare providers seeking to maintain operational efficiency and financial stability. From the initial patient engagement in pre-registration to the final steps of analytics and reporting, each phase of the RCM process plays a pivotal role in ensuring a seamless financial flow. Mastery of these steps is not just about managing finances; it's about fostering a healthcare environment where administrative efficiency and patient care go hand in hand. As the healthcare landscape continues to evolve, so does the need for robust, efficient RCM processes. Healthcare providers who excel in RCM are not only financially sound but also positioned to provide the highest quality of patient care.