In this article, we will explore some of the challenges associated with medical billing in practice management, as well as the benefits of automating your current practice management system software.

Everyone in healthcare knows receiving payments is hard. They know it’s not just one thing that makes it hard. It’s all the small, routine tasks that are never reported, all the conversations, and all the files moving between systems that are never mentioned in your monthly report, determine your budget, and help to make smarter business decisions.
Industry experts have been saying for the past five years how a surge of automation is leading to the next big change in healthcare. One example we meticulously follow is the day to day operations and financial impact of automation on medical billing and practice management.
What is a Practice Management System?
A medical practice management system is software used by large hospitals, medical offices, and group practices to manage the front end and back end of their daily operations. Some of the medical practice management features include eligibility checks, pre-authorization, payment estimation, billing and coding, payment posting, and reporting. An integrated medical practice management system like ImagineSoftware allow you to enter and track patient demographics and billing information, translate procedure codes to claims, process those claims, and receive payment from a single system. For high-volume and complex billing, automation removes some of the labor-intensive tasks, where 95% of your payment posting can be performed with no human intervention.
What is a Practice Management System Used for in a Medical Office?
Practice management systems are used to run the business side of a medical office, including scheduling, insurance claims, billing and accounting. Practice management systems typically do not include a patient’s medical records, but they can integrate with EMRs for a more robust view of a patient’s experience.
Practice Management System vs. EMR. There is some overlap between features included in an EMR versus a practice management system. EMRs focus primarily on the clinical side of a medical practice management systems focus primarily on the administrative side. Common features of an EMR include document scanning, charting, medication tracking, and appointment scheduling. Common features of a practice management system include the following:
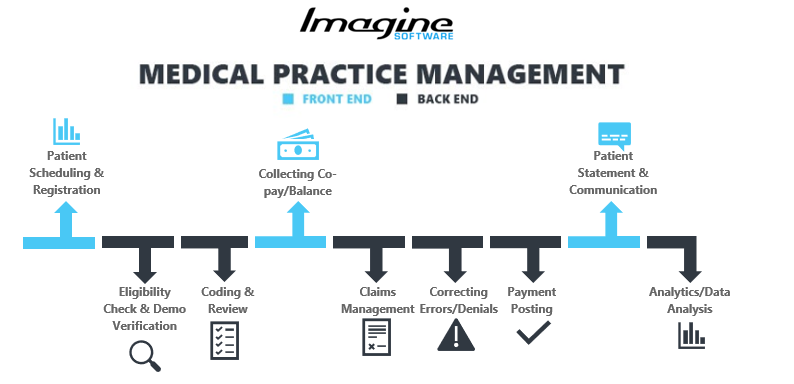
- Patient Scheduling and Registration - setting an appointment via an online portal or with the front desk; providing demographic data, updated contact details, and payer information
- Eligibility Check and Demographic Verification - including pre-authorization, instantly highlights issues with payer compatibility. Resolving these issues prior to a patient visit can reduce your denial rate later
- Coding and Review - translating medical practice diagnostics, equipment and procedures as billable records while reducing instances of denials due to incorrect or missing information
- Collection of Co-pay/Balance - the fixed amount received from a patient for a service immediately after the appointment or soon after
- Claim Management - creating, validating and submitting a claim to a clearinghouse or payer, either electronically as an e-claim or manually as a paper claim
- Correcting Errors/Denials - systematically addressing the causes of why a claim was rejected or denied before resubmitting it for consideration
- Payment Posting - posting payments into the respective patient accounts against a particular claim to reconcile them
- Patient Statement and Communication - sending patient invoices and reminders via their preferred method of contact, either over the phone, through email, or as a printed statement
- Analytics/Data Analysis - comprehensive financial dashboards can help you and your team analyze the performance of your practice at a single glance
Is it Possible for Any Existing Practice Management Systems to be Integrated with the EHR or EMR?
The short answer is, Yes. Any practice management system can theoretically be integrated with any EHR, so long as they can share data seamlessly. You’ll know if your practice management system and EHR are integrated if a patient’s medical records and insurance information are available in the same place and change one another at the same time.
For more detail, it’s important to distinguish between an integration and an interface. An interface is a feature that connects two or more independent systems, so they can communicate with data in a standard file format that’s stored in multiple locations. As such, there will often be restrictions on what information can be transmitted between the EHR and the practice management system. Data maintained in one location is usually indicative of a full integration. Instead of a patchwork of applications desperately trying to talk, the systems share a common code and database.
Integrating complex systems comes with its own social and technical challenges. Social challenges include regulatory restrictions, political constraints, and navigating operational requires of backend billing staff with front end administrative requirements. Technical challenges include building around legacy, premise systems, and cloud-based applications.
Challenges Associated with Medical Billing in Practice Management
Obstacles in implementing a medical practice management software include a lack of time to set up the infrastructure, lack of expertise, and system privacy/security:
- Security and privacy of web-based or cloud-based practice management software is a concern when hosted on another company’s server. Since this software is available from anywhere with a web connection, it’s also vulnerable to attacks by cybercriminals. Consider the financial and reputational risks related to use of third parties for core services. If security is a priority, check out ImagineMedFMTM VPN, encryption, and user authentication.
- Billing and collections, charge capture and coding was rated as one of the top risk areas for healthcare organizations in 2019. While outsourcing medical billing is a common method for offloading organizational tasks, lack of visibility into controls of third-party systems can result in lost revenue and lower claim resolve rates. Furthermore, outsourcing occasionally requires careful supervision to ensure business and patient experience standards are upheld.
- Value-based care holds a healthcare organization accountable for both the clinical and financial outcomes of a patient’s care. 36% of hospital system executives are exploring medical practice management systems that will allow them to streamline financial and clinical systems. This challenge increases exponentially for multi-specialty practices whose claims are spread out across multiple billing systems.
- Staff turnover and retaining talent affects provider workloads, patient outcomes and costs when managed using manual billing systems. Some doctors will choose employment with a healthcare system as a way to avoid the clerical responsibilities associated with running their own practice. For practice owners who remain independent, they are faced with the challenge of providing the necessary training and resources their staff needs to manage their day to day.
Benefits of Automated Practice Management System Software
Products like ImagineBillingTM built for high-volume, complex medical billing can be configured to your current practice management software workflow while automating it in the following ways:
- Real-time validation of demographic information, insurance eligibility checking, and pre-authorization makes quick work of top sources of claim denials.
- Claim generation, scrubbing and submission automatically looks for issues in your claims before they are sent to your clearinghouse or payer.
- Electronic Remittance to automatically post insurance payments and reconcile balances much faster than can be done manually.
- Real-time analytics and business intelligence gives you centralized access to business information and status reports for making smarter business decisions.